Mental health and co-occurring disorders are surprisingly common, with around 7.9 million people in the United States suffering from them. Although they occur in a large population of people, treating co-occurring diagnoses correctly can be challenging. As a result, finding a treatment center that deals specifically with mental health and co-occurring disorders is especially important to effective treatment.
What Is a Co-occurring Disorder?
If you suffer from a mental health disorder alongside a substance use disorder, it is often referred to as a co-occurring disorder or dual-diagnosis. Although the connection between addiction and mental health is fairly common knowledge among the addiction services community, the debate over the best form of treatment still survives. Because addiction and mental health often feed off each other, an interdisciplinary form of treatment is often needed. In order to best treat the co-occurring mental health and substance abuse, the treatment also needs to target both conditions at once.
Alcohol and Substance Use Disorders
According to the latest version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), alcohol and drug addictions are classified as substance use disorders. When your addiction to a substance leads to health problems and/or causes negative impacts on other aspects of life including family, work, relationships, and school, you may have a substance use disorder. For instance, risk factors of alcohol abuse and drug abuse include:
- genetics
- the type of drug
- emotional trauma
- peer pressure
- symptoms of mental illness, such as depression and anxiety disorders
- environmental stress, including seeing people in your household use
In addition, the most commonly abused forms of substances include:
Stimulants: drugs that stimulate the brain, creating a hyper-focused sense of being and high energy. Well-known stimulants include:
- cocaine
- amphetamines
- methamphetamines
Depressants: in drug form, “downers” reduce the symptoms of mental illness and help you sleep. Alcohol is also a depressant Depressant drugs include:
- barbiturates
- benzodiazepines (Xanax, Valium, Ativan)
- chloral hydrate
- paraldehyde
The 4 Stages of Addiction
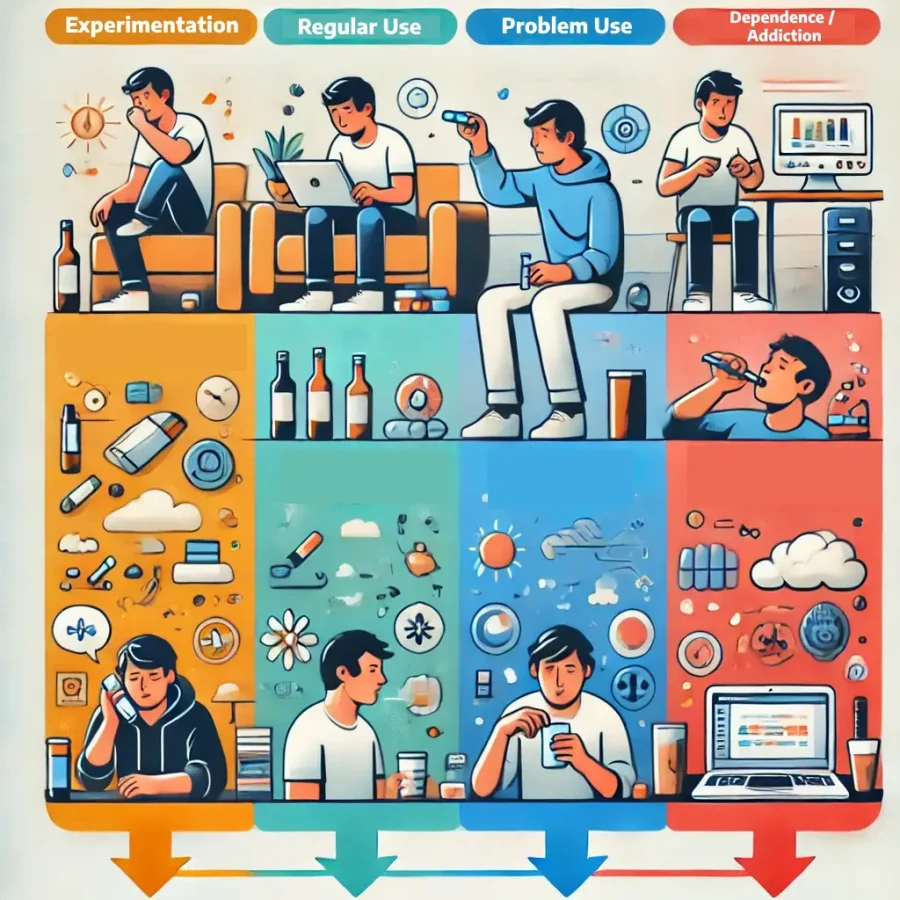
Understanding the stages of abuse can better help you understand your addiction. There are four main stages of addiction: experimentation, regular use, problem or risky use and addiction/dependence. Many experts believe using substances at a younger age increases the risk of addiction. In addition, the younger you are when you first start using, the more quickly you move through the stages.
Stage 1:
Experimentation
In teens and young adults, this initial stage usually involves using with your peers “just for fun”. Sometimes, teens start using in order to defy authority figures and rebel. However, in this stage, the use is infrequent and may be influenced by peer pressure. In adults, experimentation may be a response to external factors, such as losing a spouse or a job. Alcohol use is also normalized in adults, so experimentation is not uncommon. While some people may stop the cycle at experimentation, others go on to the next step: regular use.
Stage 2:
Regular Use
This stage involves using drugs or drinking alcohol on a regular basis, either with friends or alone. In addition, a pattern of use may begin to become obvious as well. This can include drinking on certain days (i.e. during the weekend) or drinking in predictable circumstances (i.e. when lonely, bored, or stressed).
Stage 3:
Problem Use
At this stage, your substance of choice becomes prioritized. Furthermore, risky behaviors may also develop, including but not limited to:
- isolation from current friends and family into social circles with fellow regular users
- binge drinking
- driving under the influence
- no motivation for school or work
- behavioral changes
Stage 4:
Dependence / Addiction
Once you reach this stage, you will continue to use the substance despite the negative effects it has on your body and your mind. You may need more of the substance to get high and experience withdrawal symptoms if you stop your use. Addiction is a disease and receiving treatment is vital when you are at this stage.
Connecting Mental Health and Co-occurring Disorders
Approximately 50% of those suffering from a mental health disorder will also suffer from addiction and vice versa. Additionally, 37% of alcohol abusers and 53% of drug addicts have at least one serious mental health disorder. In some cases, the mental health condition manifests first, leading to chemical dependency and symptoms of substance abuse. Other times, the substance use disorder presents first, in turn leading to anxiety disorders, depression, or other potential psychological problems.
Self-medication is very common among those who suffer from mental health and co-occurring disorders. When you self-medicate, you abuse drugs or alcohol in order to control the symptoms of a mental health disorder, often to feel “numb” or feel better. While this may feel good in the moment, it often causes problems further down the road.
For example, some common co-occurring disorders include:
- bipolar disorder and alcohol addiction
- depression and alcohol addiction
- schizophrenia and stimulant addiction
- anxiety and benzodiazepine addiction
- PTSD and drug or alcohol addiction
Mental Health and Co-Occurring Disorders Treatment:
Co-occurring disorders can be difficult to diagnose. For example, many people who seek help for substance abuse aren’t aware they have a mental health disorder until they become clean and sober. Oftentimes, this is because their mental health symptoms are masked by their addiction.
If you think you have a co-occurring mental health and substance abuse disorder, you should make sure to seek the right type of treatment. The best treatment for a co-occurring disorder is an integrated treatment model that simultaneously treats both your mental health disorder and addiction. When the two disorders are treated separately, the risk of relapse can be exceedingly high. Many facilities provide valuable dual-diagnosis inpatient and outpatient programs. Through the right combination of psychotherapy, group programs and medication, you can create a lasting recovery. In fact, many of these programs are staffed with highly-skilled, highly trained professionals who specialize in co-occurring disorders. By working together, your team can create a well-rounded treatment plan that takes into account your addiction as well as your mental health condition.
Your treatment plan should include:
- Education about addiction and mental health disorders
- Individual, group, and family therapy
- 12-step programs
- Medication management
- Relapse prevention planning
- Holistic therapies (yoga, acupuncture, meditation, etc)
- Stress management
FAQ
- What are co-occurring disorders?
Co-occurring disorders refer to the presence of both a mental health condition and a substance use disorder in the same individual. These conditions often interact, making treatment more complex. - How are co-occurring disorders treated?
Treatment typically involves integrated care, addressing both mental health and substance use disorders simultaneously. This may include therapy, medication, group counseling, and support programs. - Can someone fully recover from co-occurring disorders?
Yes, with the right treatment and ongoing support, individuals can manage their conditions effectively and lead fulfilling lives. Recovery is often a lifelong process requiring dedication and the right resources. - What therapies are commonly used to treat co-occurring disorders?
Common therapies include Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), Motivational Interviewing (MI), and trauma-informed care. These approaches help address the underlying issues of both disorders. - Why is it important to treat mental health and substance use disorders together?
Treating both conditions together ensures a comprehensive approach to recovery. Ignoring one disorder can lead to setbacks in the treatment of the other, as they are often interconnected. Integrated treatment improves overall outcomes.
We Can Help You
At The Blackberry Center, you will have the opportunity to begin the journey to lifelong recovery in our state-of-the-art facilities.
If you or one of your loved ones are struggling with addiction, we can help. We use a personalized approach to addiction treatment. Our focus is on treating the disease, not the symptoms. We put our patients first every step of the way.
Our substance abuse-only treatment programs include detox, residential and PHP. Our on-site rehab programs focus on a comprehensive recovery approach. They address your physical, mental and spiritual needs for optimal wellness.
Your needs are unique. We treat you as such.
Reach Out For Help Today
We welcome you to The Blackberry Center. From support groups to individual therapy treatment options, we are here to fight the addiction battle with you.
Reach out to us online today. You can also call us at (813) 908-4199.
